Ugh, saturated fats. Talk about one of the most polarizing nutrients in the field of nutrition sciences. Observational data questions their link to CVD (1). Original meta-analyses of RCT data that substituted PUFAs for SFA didn't adequately isolate their effects, were accused of biased inclusion and further analyses that have corrected for biases saw beneficial effects disappear and some cause for concern, regarding n-6's (2, 3,4 ) - this has been critiqued as well here and here. SFAs are just a scientific PITA. I don't personally fear consuming them - I prioritize some over others, sticking to plant varieties mostly. I personally take the perspective that if you're focusing a lot of your diet around plants, which are cardio-protective for a number of reasons (5,6), you're doing yourself some good.
One topic of scientific discussion that's come up lately, and the reason for a lack of a link between saturated fat and CVD, is the way that LDL particle subclasses and number may be more predictive of CVD than just LDL-C (7). The idea that LDL-C isn't the best predictor isn't new, as publications questioning it's ability to predict CVD outcomes/mortality have been around since the 90's (8,9). Many will cite Framingham study data to show that LDL-C is a poor predictor of CVD (see here), though the same data has been used to set up prediction models for CHD that employs LDL-C thresholds (see here) - i'm not an expert on Framingham data so feel free to comment. Still, it's been noted for 2 decades that LDL-C isn't a significant predictor of CHD morbidity/mortality in adults >70yrs old (10). More recently, LDL-C has been shown to be a poor predictor of CVD outcomes for type 1 diabetes (11). Some have even questioned whether low LDL-C is detrimental, as it has been linked to non-cardiovascular mortality, though this association is largely confounded and is an active area of research (12,13, 14). However, LDL-C has been shown to still be a decent predictor of CHD in diabetics, though i'll discuss that further below (15). I don't see LDL-C as an entirely useless number, but it's certainly not the most reliable predictor (as Dr. Mellor pointed out, it's not great in the clinic either if you have high TGs, due to the way it's calculated (41)). From my interpretation of reading the critiques of LDL-C, especially from Framingham data, it more seems to attack the idea that normal LDL-C guarantees reduced/minimal risk, not that abnormally high levels are a good thing. As more advanced techniques are applied, research is showing that LDL-C may over or underestimate the risk of future coronary events (16).
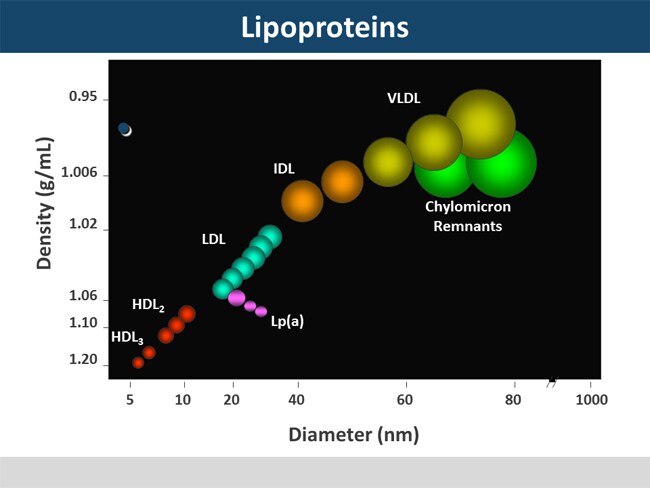
I see it quite often, that LDL particle size is the issue here - the idea that small LDL particles are more atherogenic. I've heard a number of reasons cited, in both literature and on the internet, that small LDL particles are able to more easily penetrate the intima, and have less antioxidant to protect PUFA/are more easily oxidized. While this sounds nice/pseudo-logical, it has not stood up to the research. It's the particle number, not the size - earlier research focused on the particle size, concluding that smaller LDL particles were more atherogenic. This research was limited by its methodology, using gel electrophoresis and not NMR, leaving it able to calculate average size but not number. Calculating average size leaves one with the question of whether a specific therapy (diet , statin) led to an increase in smaller particles or a decrease in larger particles - early studies suggesting small particles were more atherogenic didn't control for this inverse relationship, or their individual relationships with other CVD risk factors (17) - I highly encourage anyone interested in this topic to read this reference. Recent research, including the MESA trial (18), the Women's Health Study (19), and the Veterans Affair HDL Intervention Trail (20), has confirmed that particles, large or smaller, are equally atherogenic, when you control for particle number/confounding factors, and that past associations between small LDL/CVD were likely due to increases particle number, giving a subclass pattern B. Re-analysis of the Framingham study also showed that LDL-P number predicted future CVD events more so than LDL-C (21). LDL particle number can be quantified using NMR spectroscopy (preferred method) or immunoassay to determine ApoB concentration (primarily found in a 1:1 ratio on LDL, as well as potentially atherogenic VLDL, IDL and Lp(a)). For more reading on the importance LDL-P number, see here, .
Given that particle number is essential to quantify, and that LDL particle size appears to be less predictive of CVD risk when accounting for total particle number, this requires us to look critically at some of the diet studies that have been performed thus far.
I have a lot of questions that require further research:
1. Focusing on particle number, and not average size, what role does carbohydrate density of the diet play in the development of CVD? Many studies have focused on carbohydrates effect on LDL particle size, and only a few have quantified total number of particles. Often, the carbohydrate diet is rich in simple carbohydrates. Further research needs to look at the role of total carbohydrate density, glycemic load, total fiber and fiber types on LDL particle number.
2. How does the ratio of fatty acids play a role here? I want to see studies employing different ratios of SFA:MUFA:PUFA (mixed n-6/n-3, long and short chain).
3. How do different dietary sources of SFA affect particle number? Lumping all sources of SFA's together isn't doing a whole lot for clinicians. And even the studies that Krauss has done that use high SFA intake are only 15% of kcals. This does not condone daily bulletproof coffees or eating excessive amounts of butter.
4.Are there significant sex differences affecting particle number in response to diet therapy? Many of these studies only looked at men or women, very few looked at mixed populations.
5. What are the interactions between lipid oxidation and particle number? I would like to see changes in inflammatory molecules alongside these diet therapies. Let's not be too reductionist about risk factors.
6. Are any micronutrients having an effect on LDL-P? Krauss suggested heme iron may explain the interactions between low CHO, high SFA and beef. I would love to see the effects of choline, as it is required for LDL secretion (this was hinted at in the egg yolk study).
7. How do all non-nutritive factors (phytochemicals/antioxidants/bioactive compounds) affect LDL-P? We saw the effects of some phytochemicals with the Mediterranean diets, but I'd love to see something as simple as 2 cups of green tea per day's effect on LDL-P number. Can this mitigate potentially detrimental effects of higher simple carbohydrate consumption?
8. What's the relative effect of HDL in all of this? Although I don't think anyone is arguing that we should be on Ornish diets, or that we need to, his very low fat diet, which reduced HDL and increased TG's was still able to reverse atherosclerosis. Is looking just at serum biomarkers in isolation limited?
9. Should diets be tailored to patterns A or B of lipoprotein sublcasses? A few studies looked at these patterns but often didn't quantify total particle number - shifts in subclasses were determined by shifts in the mean particle size.
10. Study duration - most of these were 12 weeks long. We need a lot longer data
11. What's exercise doing in all of this? We know that exercise has a whole host of benefits for improving glycemic control/lipids. I saw very little discussion of exercise when comparing high carb to high fat diets.
12. What role is genotype playing here? See here and here for some preliminary data.
13. What interactions are different dietary therapies having with different statin use?
14. We need to be comparing changes in LDL-P back to reference values. I saw articles referring to LDL-P reference values from heterogeneous populations, with the 50th percentile representing 1300 nmol/L. A reduction in LDL-P by diet therapy, especially with what is seen in short-term weight loss, doesn't necessarily put someone into a safe/optimal range. I found a NMR LDL-P testing site that lists ranges of LDL-P, with less than 1000nmol as being optimal. I'm not sure if this is universally agreed upon in the literature, and the AHA guidelines don't seem to make mention of specific targets. Targeting long term diet therapy, that uses consistent methodology to analyze results, and seeing what gets us to low levels with reduced intimal thickening/CVD events is essential. Neither the study of the reduced carb diet + eggs or the Mediterranean diet saw drops in total LDL particle number to an optimal range - whether this is limited by length of study or actual diet quality is not known. Normal ApoB values can be found here. Krauss' study of HFLC and LFHC diets in healthy subjects reduced ApoB levels to intermediate ranges in both groups. There's a lot of work to be done before we start saying what is superior/inferior.
15. Are there detrimental effects to too low of an LDL-P?
This research is in its infancy. The focus on average particle size, without looking at particle number, leaves us limited in how we can apply this data to clinical nutrition. Further research is certainly needed before we go making overarching statements about what the best diet appears to be. I'm getting a bit frustrated with individuals jumping on boats before there is quality, comprehensive data. The low-carb community seems to have led the way in stating that saturated fat is benign, and that we should all be eating lower carb diets - certainly, the much-less-cited Krauss study suggesting an interaction between saturated fat and beef doesn't support the dietary paradigm that is being pushed by many. I agree, that the data so far suggests a lot of promise for low carbohydrate diets, especially for short term weight loss, but let's not jump to conclusions.
Jumping to conclusions based off of a few studies with limited methodologies and inconclusive endpoints is what leads everyone to thinking that nutrition is such a soft science. Evangelizing with preliminary data that supports your dietary paradigm is not being scientific, and it is surely not being an evidence-based practitioner. I'm going to wait until we have long term diet trials that get LDL-P number/APoB into an optimal range, helps maintain a healthy weight, has good adherence, shows normal levels of inflammatory markers, hits the DRI's for micronutrients and fiber, doesn't appear to increase risk factors for other diseases, and has some hard endpoints for CVD outcomes.
For now, let's not overcomplicate this. Maintaining a healthy weight/waist circumference, exercising, preventing diabetes, eating less simple carbohydrates and increasing fiber and plant food intake are all still good advice. Until advanced lipoprotein tests become more readily available, non-HDL cholesterol levels appear to be a good predictor of LDL-P number as determined by ApoB, though not perfect (39, 40). I can't relay my frustration enough that individuals have taken the 'saturated fat myth' and translated it to eat more butter - no one ever said don't eat butter, and the dietary guidelines even from the beginning in 1980 have stressed that we shouldn't be eliminating food groups. Dietary planning and hitting the DRI's for micronutrients are still important; this almost inherently means reducing your intake of minimally nutritious foods (added oils/fats, sugars, and refined grains). We don't have good enough data to talk about just saturated fat, as there appear to be other dietary interactions, and type of saturated fat is quite important - I've expressed before that if you're hitting the DRI for potassium and fiber, the average person probably won't be eating a high SFA diet to begin with. I have yet to see any strong data that consuming SFAs at 7-10% of total kcals has detrimental effects.
*Disclaimer: I loved reading lipid research but I'm not a lipid researcher. I surely have not covered the breadth of all that is out there in the literature. Feel free to comment with any questions/critiques.
1.http://annals.org/article.aspx?articleid=1846638
2. http://www.plosmedicine.org/article/info%3Adoi%2F10.1371%2Fjournal.pmed.1000252
3. http://ebm.bmj.com/content/15/4/108.extract
4. http://www.ncbi.nlm.nih.gov/pubmed/21118617
5.http://circ.ahajournals.org/content/123/24/2870.full
6.http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3028947/
7.http://www.aacc.org/publications/clin_chem/podcast/Documents/ClinChem_201305_Rader_McConnell.pdf
8.. http://www.ncbi.nlm.nih.gov/pubmed/1638188?dopt=Abstract
9. http://www.ncbi.nlm.nih.gov/pubmed/2144195?dopt=Abstract
10. http://jama.jamanetwork.com/article.aspx?articleid=381733
11. http://www.medscape.com/viewarticle/826982
12. http://www.ncbi.nlm.nih.gov/pubmed/1355411
13.http://www.medscape.com/viewarticle/760891
14. http://www.ncbi.nlm.nih.gov/pubmed/21285406
15. http://atvb.ahajournals.org/content/20/3/830.long
16. http://circ.ahajournals.org/content/129/5/553.abstract
17.http://circ.ahajournals.org/content/119/17/2396.full
18.http://www.ncbi.nlm.nih.gov/pubmed/16765964?dopt=Abstract
19. http://circ.ahajournals.org/content/119/7/931.abstract
20. http://circ.ahajournals.org/content/113/12/1556.abstract
21. http://www.ncbi.nlm.nih.gov/pubmed/19657464
22.http://www.ncbi.nlm.nih.gov/pubmed/24099723
23. http://www.fasebj.org/content/28/1_Supplement/249.8
24. http://ajcn.nutrition.org/content/67/5/828.short
25. http://ajcn.nutrition.org/content/83/5/1025.long
26. http://jn.nutrition.org/content/141/12/2180.full
27.https://www.ncbi.nlm.nih.gov/pubmed/24445969
28.https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2952573/
29. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2889993/
30. http://www.ncbi.nlm.nih.gov/pubmed/23021013
31. http://jn.nutrition.org/content/132/7/1879.long
32. http://www.nutritionandmetabolism.com/content/5/1/29
33. http://www.ncbi.nlm.nih.gov/pubmed/21944261
34. http://ajcn.nutrition.org/content/76/2/351.long
35. http://ajcn.nutrition.org/content/54/4/678.abstract
36. http://www.plosone.org/article/info%3Adoi%2F10.1371%2Fjournal.pone.0090863
37. http://www.jmnn.org/article.asp?issn=2278-019X;year=2014;volume=3;issue=1;spage=39;epage=44;aulast=Palazhy
38. http://www.biomedexperts.com/Abstract.bme/17145217/Heterogeneity_of_low-density_lipoprotein_particle_number_in_patients_with_type_2_diabetes_mellitus_and_low-density_lipop
39. http://circ.ahajournals.org/content/112/22/3375.abstract
40.http://www.ncbi.nlm.nih.gov/pubmed/11386890
41. http://www.ncbi.nlm.nih.gov/pubmed/23524048
42. http://www.ajcn.org/cgi/pmidlookup?view=long&pmid=12716665
One topic of scientific discussion that's come up lately, and the reason for a lack of a link between saturated fat and CVD, is the way that LDL particle subclasses and number may be more predictive of CVD than just LDL-C (7). The idea that LDL-C isn't the best predictor isn't new, as publications questioning it's ability to predict CVD outcomes/mortality have been around since the 90's (8,9). Many will cite Framingham study data to show that LDL-C is a poor predictor of CVD (see here), though the same data has been used to set up prediction models for CHD that employs LDL-C thresholds (see here) - i'm not an expert on Framingham data so feel free to comment. Still, it's been noted for 2 decades that LDL-C isn't a significant predictor of CHD morbidity/mortality in adults >70yrs old (10). More recently, LDL-C has been shown to be a poor predictor of CVD outcomes for type 1 diabetes (11). Some have even questioned whether low LDL-C is detrimental, as it has been linked to non-cardiovascular mortality, though this association is largely confounded and is an active area of research (12,13, 14). However, LDL-C has been shown to still be a decent predictor of CHD in diabetics, though i'll discuss that further below (15). I don't see LDL-C as an entirely useless number, but it's certainly not the most reliable predictor (as Dr. Mellor pointed out, it's not great in the clinic either if you have high TGs, due to the way it's calculated (41)). From my interpretation of reading the critiques of LDL-C, especially from Framingham data, it more seems to attack the idea that normal LDL-C guarantees reduced/minimal risk, not that abnormally high levels are a good thing. As more advanced techniques are applied, research is showing that LDL-C may over or underestimate the risk of future coronary events (16).
I see it quite often, that LDL particle size is the issue here - the idea that small LDL particles are more atherogenic. I've heard a number of reasons cited, in both literature and on the internet, that small LDL particles are able to more easily penetrate the intima, and have less antioxidant to protect PUFA/are more easily oxidized. While this sounds nice/pseudo-logical, it has not stood up to the research. It's the particle number, not the size - earlier research focused on the particle size, concluding that smaller LDL particles were more atherogenic. This research was limited by its methodology, using gel electrophoresis and not NMR, leaving it able to calculate average size but not number. Calculating average size leaves one with the question of whether a specific therapy (diet , statin) led to an increase in smaller particles or a decrease in larger particles - early studies suggesting small particles were more atherogenic didn't control for this inverse relationship, or their individual relationships with other CVD risk factors (17) - I highly encourage anyone interested in this topic to read this reference. Recent research, including the MESA trial (18), the Women's Health Study (19), and the Veterans Affair HDL Intervention Trail (20), has confirmed that particles, large or smaller, are equally atherogenic, when you control for particle number/confounding factors, and that past associations between small LDL/CVD were likely due to increases particle number, giving a subclass pattern B. Re-analysis of the Framingham study also showed that LDL-P number predicted future CVD events more so than LDL-C (21). LDL particle number can be quantified using NMR spectroscopy (preferred method) or immunoassay to determine ApoB concentration (primarily found in a 1:1 ratio on LDL, as well as potentially atherogenic VLDL, IDL and Lp(a)). For more reading on the importance LDL-P number, see here, .
Given that particle number is essential to quantify, and that LDL particle size appears to be less predictive of CVD risk when accounting for total particle number, this requires us to look critically at some of the diet studies that have been performed thus far.
- For starters, and as would be expected, reducing trans fat in the diet has been shown to reduce LDL-P number (22). No surprises here.
- Avocado consumption was recently shown to reduce LDL-P in overweight and obese men and women in the 25th-90th percentile of LDL-C (23).
- Dr. Krauss showed a while back that saturated fat increases LDL size- this study did not, however, look at LDL-P or quantify ApoB (24).
- Krauss' 4wk study of weight loss (25) in obese men showed a linear effect of reducing carbohydrate content on LDL particle size. This study did measure ApoB, and the lowest carbohydrate content (26%) saw the greatest reduction in ApoB - the differences between the lower (8%) and higher (15%) were not statistically significant, although the raw reduction in ApoB was greater for the lower saturated fat (just lists as NS difference, no value to see if it was trending towards significance). In the second part of the study inducing weight loss, there were further favorable ApoB reductions, with the greatest effect for the highest carbohydrate content (54%), and a slight increase in ApoB for the lowest CHO/SFA content, though this was not significant from the slight decrease seen in the lowest CHO/high SFA diet.
- Krauss followed up on this previous observation with a study (26) looking at the effect of increasing dietary protein in place of CHO with varied SFA intake - their results slightly contradicted the previous study, with the low CHO high SFA diet resulting in a trend toward increasing LDL particle concentrations across all subclasses. The low CHO low SFA saw the greatest reduction in ApoB. The difference between this and the last study was that this study, while still getting most of its SFA from dairy, got most of its protein from beef. Their results suggest some sort of interaction between SFA and another component of beef, and conclude that the benefits of a low CHO diet that includes beef are only seen in the context of low SFA intake. Of note, this study did not induce weight loss and males had to meet a criteria of having a BMI of greater than 20 and less than 35.
- Another study by Krauss' group (28) looked at the effects of a LCHF vs HCLF diets on Lp(a) and oxidized lipoproteins during weight maintenance, showing a beneficial effect of LCHF. The study showed a reduction in triglycerides, ApoB, oxidized phospholipids/ApoB, and Lp(a) for the LCHF diet. Note that this LCHF diet that showed improvements was almost 14% PUFA (higher than the recommended 10%), and 13% saturated fat (not much higher than the 10% threshold). Also of note, the LFHC diet was half simple carbs, half complex (I didn't see total fiber data reported).
- Another study (29) looked at the effects of reduced carb (RC) or reduced fat (RF) diets during weight maintenance after significant weight loss on subclasses of lipoproteins. They found mild 'improvements' in lipid subclasses, and the study did not list total ApoB/particle number. The study was severely limited in that the reduced carb group had higher intake of carbs than directed, and the reduced fat group had higher energy intake than the reduced carb.
- A recent RCT (30) looking at a carb reduced diet with egg consumption, with or without the yolk, showed a decrease in total LDL particles across 12 weeks, as well as Oxidized LDL for both treatments, with the yolk group seeing a greater decrease in LDL particle number, and the without group seeing a greater decrease in Oxidized LDL. ApoB was reduced for both treatments, with a greater effect for those consuming the yolk. While this RCT occurred during weight loss, the greater effects seen for the reduction in LDL particle number for yolk consumption lends itself to a promising and beneficial effect of yolk consumption.
- There was an interesting study (31) looking at the effects of a ketogenic diet on lipids and lipid subclasses in normal weight men. The study didn't look at total particle number, just subclass diameter changes. And while it looks promising, the subjects did lose weight, enough to predict changes in HDL and TAG. The study also looked at the effects of the ketogenic diets on individuals who had patterns A or B distributions to begin with, showing a more pronounced effect for shifting LDL subclasses from a pattern B to pattern A style, though they still did not report total LDL particle number, just mean particle size. I'm a bit skeptical of this study though, because they say it's ketogenic and the individuals reported BHB concentrations, but the ketogenic diet was 30% protein - I'm not sure how one stays in ketosis with that high of a protein intake, especially whey protein, though them losing weight probably played into this (i'm not a ketosis expert, feel free to comment).
- It might seem like low carb diets are shining through as the clear winner here. However, two studies of Mediterranean style diets have shown promising results. The first (32) saw weight loss with a typical Mediterranean diet and one supplemented with several phytochemicals in individuals with hypercholesteremia and Metabolic Syndrome. The supplementation group saw greater weight loss, better improvements in TGs and HDL, and a greater reduction in ApoB. Both diet groups saw considerable decreases in energy, increases in fiber, mild reduction in carbohydrates (still much above the keto threshold), major reductions in SFAs (30-35 grams down to about 10-15). The second study (33) also looked at the effects of a mediterranean style diet in females with metabolic syndrome. It also reported reductions in ApoB for both groups, with a greater effect for those receiving the medical food (Med + phytosterols/chemicals). These results are confounded by weight loss, however, but do warrant further studies of the Mediterranean diet's (moderate complex carb, low SFA) effectiveness for reducing LDL particle number in normal weight individuals. I'd love to see a well controlled, weight stable, matched face off of Mediterranean diets and Low Carbs.
- A rather interesting study (34) looked at the effect of high fiber oat vs wheat cereal consumption on lipid subclasses and lipid particle number. Both groups gained some weight weight (on avg about a 1lb), but the high fiber oat group decreased total LDL-P number, whereas the wheat group slightly increased. Both groups increased their fiber intake by about 10g, and increased carbohydrates by about 5% and reduced fat by about 5%, increasing the PUFA:SFA ratio. This isn't the first time this has been shown - a previous study (35) looking at supplementation with wheat or oat bran showed a significant decrease in ApoB after oat bran supplementation but not after wheat bran. This is likely speaking to the role that soluble fiber plays in effecting LDL-P number.
- Other supplements may play a role in decreasing LDL-P number, with a recent study (36) in high fat fed Zucker rats showing a reduction in LDL-P number after supplementation with alpha-lipoic acid (a component of the pyruvate dehydrogenase complex). They cite several mechanisms, including a reduction in fatty acid synthase - i'm skeptical of the rat model due to their differences in DNL.
- A study (37) looking at the effects of coconut vs safflower oil in healthy controls and diabetics did not find differences in ApoB concentrations for the healthy controls. ApoB levels were higher in both groups of diabetics. The study was poorly controlled and I wouldn't take much from it.
- There is considerable heterogeneity in LDL-P number among individuals with T2DM, and even achieving LDL-C less than 100mg/dL can still leave individuals with significantly different LDL-P numbers (38)
- Looking back to 2003, Mensink et al (42), performed a meta-analysis of 60 randomized trials in weight stable individuals. In table 1, they list their results for replacement of 1% of dietary energy from carbs with different fatty acids. The results showed an average increase replacing carbs with SFAs, large decreases for MUFAs and even larger for PUFAs. It should be noted that there was a decent range in the total ApoB changes when replacing carbs with SFAs, some seeing a reduction in the number. However, this reduction was still significantly less substantial than replacing carbohydrates with MUFAs/PUFAs.
 |
| Credit: Berkley Heart Lab |
I have a lot of questions that require further research:
1. Focusing on particle number, and not average size, what role does carbohydrate density of the diet play in the development of CVD? Many studies have focused on carbohydrates effect on LDL particle size, and only a few have quantified total number of particles. Often, the carbohydrate diet is rich in simple carbohydrates. Further research needs to look at the role of total carbohydrate density, glycemic load, total fiber and fiber types on LDL particle number.
2. How does the ratio of fatty acids play a role here? I want to see studies employing different ratios of SFA:MUFA:PUFA (mixed n-6/n-3, long and short chain).
3. How do different dietary sources of SFA affect particle number? Lumping all sources of SFA's together isn't doing a whole lot for clinicians. And even the studies that Krauss has done that use high SFA intake are only 15% of kcals. This does not condone daily bulletproof coffees or eating excessive amounts of butter.
4.Are there significant sex differences affecting particle number in response to diet therapy? Many of these studies only looked at men or women, very few looked at mixed populations.
5. What are the interactions between lipid oxidation and particle number? I would like to see changes in inflammatory molecules alongside these diet therapies. Let's not be too reductionist about risk factors.
6. Are any micronutrients having an effect on LDL-P? Krauss suggested heme iron may explain the interactions between low CHO, high SFA and beef. I would love to see the effects of choline, as it is required for LDL secretion (this was hinted at in the egg yolk study).
7. How do all non-nutritive factors (phytochemicals/antioxidants/bioactive compounds) affect LDL-P? We saw the effects of some phytochemicals with the Mediterranean diets, but I'd love to see something as simple as 2 cups of green tea per day's effect on LDL-P number. Can this mitigate potentially detrimental effects of higher simple carbohydrate consumption?
8. What's the relative effect of HDL in all of this? Although I don't think anyone is arguing that we should be on Ornish diets, or that we need to, his very low fat diet, which reduced HDL and increased TG's was still able to reverse atherosclerosis. Is looking just at serum biomarkers in isolation limited?
9. Should diets be tailored to patterns A or B of lipoprotein sublcasses? A few studies looked at these patterns but often didn't quantify total particle number - shifts in subclasses were determined by shifts in the mean particle size.
10. Study duration - most of these were 12 weeks long. We need a lot longer data
11. What's exercise doing in all of this? We know that exercise has a whole host of benefits for improving glycemic control/lipids. I saw very little discussion of exercise when comparing high carb to high fat diets.
12. What role is genotype playing here? See here and here for some preliminary data.
13. What interactions are different dietary therapies having with different statin use?
14. We need to be comparing changes in LDL-P back to reference values. I saw articles referring to LDL-P reference values from heterogeneous populations, with the 50th percentile representing 1300 nmol/L. A reduction in LDL-P by diet therapy, especially with what is seen in short-term weight loss, doesn't necessarily put someone into a safe/optimal range. I found a NMR LDL-P testing site that lists ranges of LDL-P, with less than 1000nmol as being optimal. I'm not sure if this is universally agreed upon in the literature, and the AHA guidelines don't seem to make mention of specific targets. Targeting long term diet therapy, that uses consistent methodology to analyze results, and seeing what gets us to low levels with reduced intimal thickening/CVD events is essential. Neither the study of the reduced carb diet + eggs or the Mediterranean diet saw drops in total LDL particle number to an optimal range - whether this is limited by length of study or actual diet quality is not known. Normal ApoB values can be found here. Krauss' study of HFLC and LFHC diets in healthy subjects reduced ApoB levels to intermediate ranges in both groups. There's a lot of work to be done before we start saying what is superior/inferior.
15. Are there detrimental effects to too low of an LDL-P?
This research is in its infancy. The focus on average particle size, without looking at particle number, leaves us limited in how we can apply this data to clinical nutrition. Further research is certainly needed before we go making overarching statements about what the best diet appears to be. I'm getting a bit frustrated with individuals jumping on boats before there is quality, comprehensive data. The low-carb community seems to have led the way in stating that saturated fat is benign, and that we should all be eating lower carb diets - certainly, the much-less-cited Krauss study suggesting an interaction between saturated fat and beef doesn't support the dietary paradigm that is being pushed by many. I agree, that the data so far suggests a lot of promise for low carbohydrate diets, especially for short term weight loss, but let's not jump to conclusions.
Jumping to conclusions based off of a few studies with limited methodologies and inconclusive endpoints is what leads everyone to thinking that nutrition is such a soft science. Evangelizing with preliminary data that supports your dietary paradigm is not being scientific, and it is surely not being an evidence-based practitioner. I'm going to wait until we have long term diet trials that get LDL-P number/APoB into an optimal range, helps maintain a healthy weight, has good adherence, shows normal levels of inflammatory markers, hits the DRI's for micronutrients and fiber, doesn't appear to increase risk factors for other diseases, and has some hard endpoints for CVD outcomes.
For now, let's not overcomplicate this. Maintaining a healthy weight/waist circumference, exercising, preventing diabetes, eating less simple carbohydrates and increasing fiber and plant food intake are all still good advice. Until advanced lipoprotein tests become more readily available, non-HDL cholesterol levels appear to be a good predictor of LDL-P number as determined by ApoB, though not perfect (39, 40). I can't relay my frustration enough that individuals have taken the 'saturated fat myth' and translated it to eat more butter - no one ever said don't eat butter, and the dietary guidelines even from the beginning in 1980 have stressed that we shouldn't be eliminating food groups. Dietary planning and hitting the DRI's for micronutrients are still important; this almost inherently means reducing your intake of minimally nutritious foods (added oils/fats, sugars, and refined grains). We don't have good enough data to talk about just saturated fat, as there appear to be other dietary interactions, and type of saturated fat is quite important - I've expressed before that if you're hitting the DRI for potassium and fiber, the average person probably won't be eating a high SFA diet to begin with. I have yet to see any strong data that consuming SFAs at 7-10% of total kcals has detrimental effects.
*Disclaimer: I loved reading lipid research but I'm not a lipid researcher. I surely have not covered the breadth of all that is out there in the literature. Feel free to comment with any questions/critiques.
1.http://annals.org/article.aspx?articleid=1846638
2. http://www.plosmedicine.org/article/info%3Adoi%2F10.1371%2Fjournal.pmed.1000252
3. http://ebm.bmj.com/content/15/4/108.extract
4. http://www.ncbi.nlm.nih.gov/pubmed/21118617
5.http://circ.ahajournals.org/content/123/24/2870.full
6.http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3028947/
7.http://www.aacc.org/publications/clin_chem/podcast/Documents/ClinChem_201305_Rader_McConnell.pdf
8.. http://www.ncbi.nlm.nih.gov/pubmed/1638188?dopt=Abstract
9. http://www.ncbi.nlm.nih.gov/pubmed/2144195?dopt=Abstract
10. http://jama.jamanetwork.com/article.aspx?articleid=381733
11. http://www.medscape.com/viewarticle/826982
12. http://www.ncbi.nlm.nih.gov/pubmed/1355411
13.http://www.medscape.com/viewarticle/760891
14. http://www.ncbi.nlm.nih.gov/pubmed/21285406
15. http://atvb.ahajournals.org/content/20/3/830.long
16. http://circ.ahajournals.org/content/129/5/553.abstract
17.http://circ.ahajournals.org/content/119/17/2396.full
18.http://www.ncbi.nlm.nih.gov/pubmed/16765964?dopt=Abstract
19. http://circ.ahajournals.org/content/119/7/931.abstract
20. http://circ.ahajournals.org/content/113/12/1556.abstract
21. http://www.ncbi.nlm.nih.gov/pubmed/19657464
22.http://www.ncbi.nlm.nih.gov/pubmed/24099723
23. http://www.fasebj.org/content/28/1_Supplement/249.8
24. http://ajcn.nutrition.org/content/67/5/828.short
25. http://ajcn.nutrition.org/content/83/5/1025.long
26. http://jn.nutrition.org/content/141/12/2180.full
27.https://www.ncbi.nlm.nih.gov/pubmed/24445969
28.https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2952573/
29. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2889993/
30. http://www.ncbi.nlm.nih.gov/pubmed/23021013
31. http://jn.nutrition.org/content/132/7/1879.long
32. http://www.nutritionandmetabolism.com/content/5/1/29
33. http://www.ncbi.nlm.nih.gov/pubmed/21944261
34. http://ajcn.nutrition.org/content/76/2/351.long
35. http://ajcn.nutrition.org/content/54/4/678.abstract
36. http://www.plosone.org/article/info%3Adoi%2F10.1371%2Fjournal.pone.0090863
37. http://www.jmnn.org/article.asp?issn=2278-019X;year=2014;volume=3;issue=1;spage=39;epage=44;aulast=Palazhy
38. http://www.biomedexperts.com/Abstract.bme/17145217/Heterogeneity_of_low-density_lipoprotein_particle_number_in_patients_with_type_2_diabetes_mellitus_and_low-density_lipop
39. http://circ.ahajournals.org/content/112/22/3375.abstract
40.http://www.ncbi.nlm.nih.gov/pubmed/11386890
41. http://www.ncbi.nlm.nih.gov/pubmed/23524048
42. http://www.ajcn.org/cgi/pmidlookup?view=long&pmid=12716665
http://journals.cambridge.org/action/displayAbstract is not a valid link.
ReplyDeleteOtherwise, great article!
Hi Gerard,
DeleteThanks for pointing that out - it's been fixed!
-Best,
Kevin
Very interesting, thank you! I'm going to look through all your references.
ReplyDeleteWhen you mention that LDL-C may be a poor predictor of risk, remember that it still may be a significant causal factor in atherogenesis. «The causes of vascular disease are weak risk factors for vascular disease» (http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3244267/). LDL-C may also have been underestimated when using the Friedewald equation. And according to a recent paper by Varbo et al., LDL-c causes IHD in abscense of inflammation (http://circ.ahajournals.org/content/128/12/1298.short).
Hi Erik,
DeleteThanks,and thanks for the links! I look forward to reading them, especially the Varbo, hadn't read it yet. I certainly agree that LDL-C is playing a major causative role - actually had some twitter chat about that and the role of HDL in all of this. I had put a link to the Friedewald equation dilemma but it wasn't highlighting, added a citation for it now!
-Best,
KCK
Hi Kevin,
ReplyDeleteFirst off, I came across your site and wanted to say thanks for providing a great heart-healthy resource to the community.
I thought you might find this article helpful to your readers who are trying to lower their cholesterol, as it shows photos of what 100% of your daily value of cholesterol looks like. It’s quite shocking! http://www.healthline.com/health/high-cholesterol/daily-value
Naturally, I’d be delighted if you share this article on http://nutrevolve.blogspot.com/2014/07/saturated-fat-particles-and-cvd.html , and/or share it with your followers on social to help them make better food choices. Either way, keep up the great work Kevin!
All the best,
Nicole Lascurain | Assistant Marketing Manager
p: 415-281-3100 | e: nicole.lascurain@healthline.com
Healthline
660 Third Street, San Francisco, CA 94107
www.healthline.com | @Healthline